Going on an Ultrasound Foreign Body Hunt
The Emergency Foreign Body Hunt
3 min read
.jpg) Fred Gromalak, DVM
:
Mar 14, 2025 4:56:44 PM
Fred Gromalak, DVM
:
Mar 14, 2025 4:56:44 PM
When facing a challenging gastrointestinal case, the power of collaboration cannot be overstated. In this recent case, a 1-year and 7-month-old spayed female Mini Dachshund presented at an emergency clinic with significant gastric distention, regurgitation, and concerns about a possible gastrointestinal obstruction.
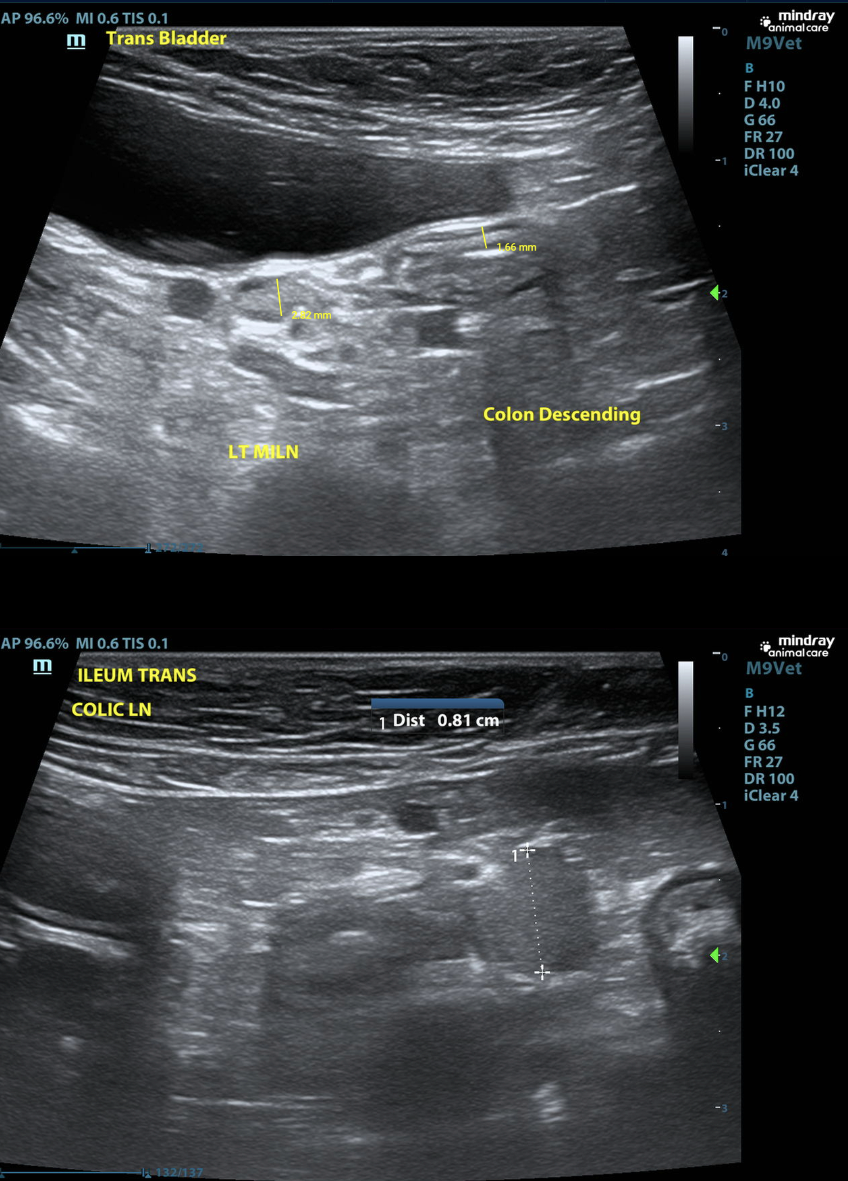
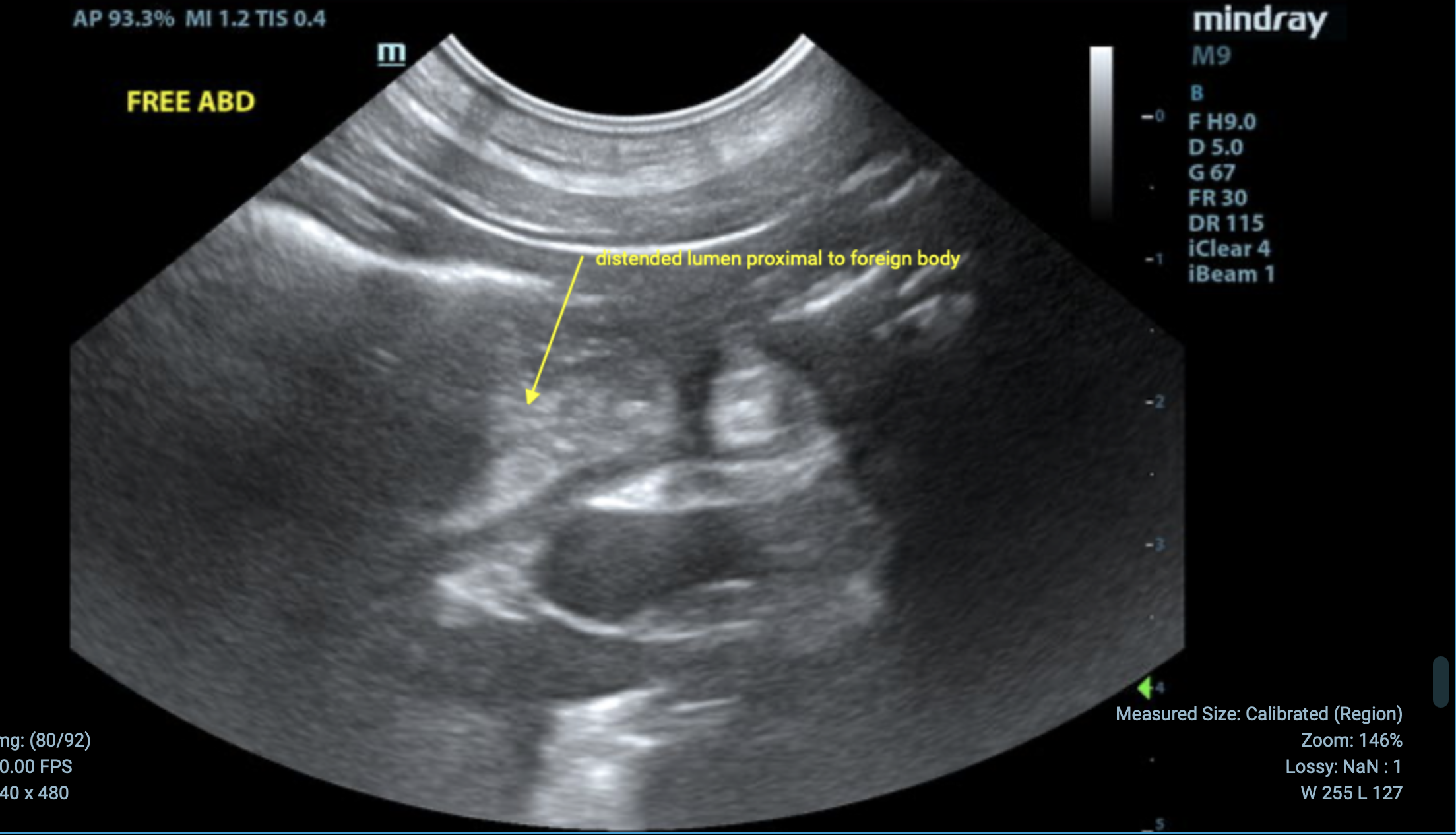
The patient had undergone an initial ultrasound exam the previous day, which revealed an ileal foreign body prompting a STAT multi-modality (ultrasound and radiograph) review by the SVS Imaging team. By leveraging the expertise of both a SVS Imaging radiologist and internist, we were able to provide a detailed and actionable care plan.

Gastric distention; rule out functional ileus/atony secondary to pain or inflammation (gastritis, ulceration, peritonitis, pancreatitis).
No gastric foreign material or outflow obstruction is identified on this study.
Nasogastric tube placement to reduce distention and discomfort is recommended.
Continue medical management for nonspecific gastroenteritis.
Consider snap cPLI testing to assess for pancreatitis, even if sonographically normal.
If the patient continues to decline, consider barium study or abdominal CT.



This case exemplifies the synergy between veterinary imaging and clinical
expertise.

About SVS Imaging
Veterinary Teleradiology and Internal Medicine Consultations: Veterinarians worldwide can rely on our specialists' expertise in interpreting RADS, CT scans, MRIs, and ultrasound images, and providing you with accurate and comprehensive diagnoses. Click here to learn more.
The Emergency Foreign Body Hunt

Road warriors of the Veterinary Field In the dynamic realm of veterinary medicine, there's a hidden gem that's gaining significant traction - the...

When you first step onto a golf course, the swing feels unnatural. You’re told to hold the club a certain way, position your feet just right, and...